How to Qualify for Wegovy, Zepbound, or Saxenda
How to Qualify for Wegovy, Zepbound, or Saxenda
Introduction
Weight loss medications like Wegovy, Zepbound, and Saxenda are changing the way doctors treat obesity. These drugs help people lose 10% to over 20% of their body weight—but they’re prescription-only and not handed out casually.
In this guide, you’ll learn the medical criteria you must meet to qualify for Wegovy, Zepbound, or Saxenda—and tips to help you work with your doctor and insurance to access these life-changing treatments.
Why Are Qualifications Required?
These medications are:
- Expensive (over $1,000/month without insurance)
- Potent (impacting hormones that regulate appetite and metabolism)
- Intended for medical obesity treatment, not cosmetic weight loss
✅ Strict qualifications ensure they’re prescribed safely to people who truly benefit.
Basic Qualification Rules
Medication | Approved Use | Minimum Criteria |
Wegovy | Weight loss (obesity/overweight) | BMI ≥30 or BMI ≥27 + condition |
Zepbound | Weight loss (obesity/overweight) | BMI ≥30 or BMI ≥27 + condition |
Saxenda | Weight loss (obesity/overweight) | BMI ≥30 or BMI ≥27 + condition |
✅ The FDA uses the same criteria for all three medications.
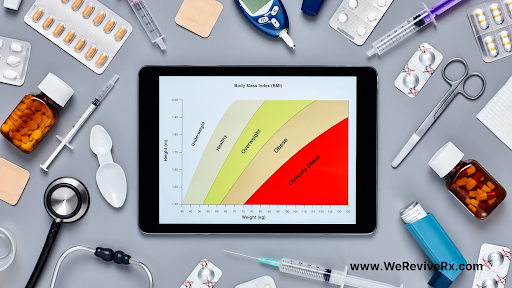
What Does BMI Mean for Qualification?
- BMI ≥30 = Automatically qualifies (obese category)
- BMI ≥27 + one or more weight-related conditions qualifies too
Examples of qualifying conditions:
- Type 2 diabetes
- High blood pressure (hypertension)
- High cholesterol (dyslipidemia)
- Obstructive sleep apnea
- Insulin resistance or prediabetes
- PCOS (polycystic ovary syndrome)
A single comorbidity paired with a BMI of 27–29.9 is enough to qualify.
How to Prepare for Your Doctor Visit
✅ 1. Know Your BMI
Calculate your BMI using an online tool before your appointment. Bring the number with you.
✅ 2. Gather Medical History
Have records of:
- Diagnosed conditions (like hypertension or diabetes)
- Past weight loss attempts (diet, exercise, programs)
- Family history of obesity or metabolic disease
✅ 3. Be Ready to Discuss Lifestyle Efforts
Some insurance companies require documentation that you’ve attempted lifestyle changes before approving medication.
✅ 4. Ask for Documentation
Make sure your doctor notes your BMI, comorbidities, and medical necessity clearly in your chart and insurance paperwork.
What About Insurance Approval?
Insurance companies often require:
- A prior authorization (PA) from your doctor
- Proof you meet FDA-approved criteria
- Evidence you’ve tried and failed conservative treatments (e.g., weight loss diet)
📌 Tip: If you are denied coverage initially, you have the right to appeal with supporting documentation.
💡 Apply for savings programs while your PA is pending:
Can You Qualify Without Diabetes?
Absolutely.
You do NOT need to have diabetes to qualify for Wegovy, Zepbound, or Saxenda.
A high BMI alone, or a moderate BMI plus a health condition, is enough.
These medications are for managing obesity—a chronic disease in its own right—not just diabetes.
What If You Don’t Meet the Criteria?
If you don’t meet the strict BMI or comorbidity guidelines, options may include:
- Lifestyle coaching programs (e.g., Noom, WW, Found Health)
- Telehealth weight loss services that offer lower-dose GLP-1 medications off-label
- Future re-evaluation if your BMI changes
Always discuss alternative strategies with your healthcare provider.
Final Thoughts
Qualifying for Wegovy, Zepbound, or Saxenda is very achievable if you meet the established medical criteria. These treatments can offer life-changing benefits—but they must be used safely, responsibly, and with medical oversight.
✔️ Know your BMI and medical history
✔️ Work closely with your provider
✔️ Be proactive with insurance paperwork and appeals if needed
📌 For downloadable BMI calculators, PA forms, and tips on insurance approval, visit our Weight Loss Prescription Center.
